52 yr old male with complaint of chest discomfort since 3 months
This is an online e log book to discuss our patient identified health data shared after taking his/her guardian signed informed consent. Here we discuss our individual patient problems through a series of inputs from available global online community of experts with a aim to solve those patients clinical problem with collective current best evidence based inputs.This blog also reflects my patient centered online learning portfolio and valuable inputs on the comments box is welcome.I have been given this case to solve in an attempts to understand the topic of patient clinical data analysis, to develop my competency in reading and comprehending clinical data including history, clinical finding, investigation.
The patient has been fully informed about his medical data being used for an online learning portfolio and his identity is fully concealed from the online viewers of this blog
Intern : N Joshua Paul
15/9/23
Chief complaints : 52 yr old male came in with the chief complaint of breathlessness since 3 months
HOPI :
A 52 yr old male, woodcutter by occupation and a resident of suryapet presented to the opd with the chief complaint of breathlessness NYHA class since 3 months, which was more during the nights or evenings than in mornings.
H/o orthopnea, seasonal variation present. It was not associated with chest pain/PND/Syncope.
No H/o burning micturition/oliguria/pedal edema//palpitations/abdominal pain/nausea/fever/diarrhoea
It is sometimes associated with excessive sweating + not associated with chest pain/palpitations/breathlessness
PAST HISTORY :
Patient developed vitiligo 10yrs ago with areas of hyperpigmentation, hypopigmentation and depigmentation.



A keloid scar on chest post CABG

 On 4 episodes of palpitations and sweating in a period of 3 months he sought for consultation CAD-TVD S/p - CABG 3 Grafts @ 2021 November
N/K/C/O HTN/DM2/Epilepsy/TB/CVA/Thyroid disorders/Asthma
TREATMENT HSITORY : treated for CAD-TVD in 2021 November
PERSONAL HISTORY : married
Occupation - woodcutter
Appetite - normal
Non vegetarian
Chronic Alcoholic used to be regular but stopped the intake 4yrs ago
Family history: insignificant
PHYSICAL EXAMINATION:
A. GENERAL EXAMINATION :
Pallor - no
Icterus - no
Cyanosis - no
Clubbing - grade 1


Lymphadenopathy - no
Odema of feet - present bilaterally grade 2 up to knee, pitting type
Raised JVP
 
Vitals :
Pr - 84 bpm
Bp - 130/80 mmhg
RR - 19 cpm
GRBS - 154 mg%
SYSTEMIC EXAMINATION :
CVS : No thrills
Cardiac sounds - S1 & S2 heard
Visible raised JVP
RS : Dyspnoea : orthopnea +, NYHA grade 1
Position of trachea : central
Breath sounds : vesicular
Adventitious sounds : b/l rhonchi + in Infrascapular, interscapular and infraaxillary area
B/L airway entry present
P/A : Soft, non tender abdomen, bowel sounds heard and no organomegaly observed
CNS : No FND
HMF - intact
Sensory system - normal
Motor system - Normal
No focal neurological deficits
INVESTIGATIONS :
2D echo:
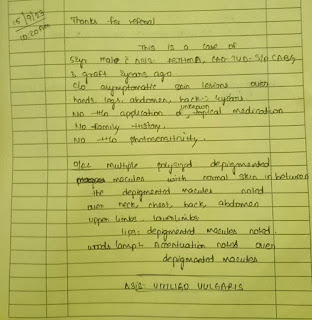
The patient was referred to dermatology department in view of vitiligo and cross consultation was done


Diagnosis : 1. Asthma
2. CAD-TVD - s/p CABG - TRIPLE GRAFT (2yrs ago)
C/o breathlessness of grade 1 NYHA
Treatment : 1. Tab. ECOSPORIN 75mg po H/S
2. Tab. MET-XL 12.5 PO/OD (at afternoon)
3. Tab. ROSUVASTATIN 20mg po H/S (at night)
4. INHALER BECLOMETHASONE DIPROPIONATE 200 mg/ sos





















Comments
Post a Comment