This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient-centred online learning portfolio and your valuable inputs on the comment box is welcome."I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
A 67yr old male who is a resident of Nakrekal and Farmer by occupation came to medicine OPD with
CHIEF COMPLAINTS:
C/O bloating of abdomen since 1 week
SOB since 1week
Decreased urine output since 15days
HISTORY OF PRESENTING ILLNESS:
Patient was apparently asymptomatic 15days ago then he developed fever which is high grade,associated with chills and rigors,associated with decreased urine output for which he was admitted in a local hospital and was given IV fluids and developed anasarca and was shifted to other hospital and foleys catheterisation was done and urine output has increased.
Patient has c/o bloating of abdomen,not associated with food intake,belchings,regurgitations but associated with SOB.
C/o B/L pedal edema — on and off , increases with prolonged sitting/standing since 15days.
Gangrene of right 3rd toe since 1month.
No c/o pain abdomen,loose stools,vomitings,cough,cold.
No c/o chest pain,palpitations,orthopnea,PND.
PAST HISTORY:
H/O gangrene and amputation of right big toe 2yrs ago.
K/C/O DM2 since 12yrs and on insulin mixtard— 30U in the morning and 25U in the evening.
N/K/C/O HRN, CAD , CVA , TB , Epilepsy , Asthma , Thyroid disorders.
TREATMENT HISTORY:
Insulin mixtard for DM
H/o blood transfusion 4yrs back (1 PRBC)
PERSONAL HISTORY:
Diet- mixed
Appetite- decreased since 20 days
Bowel and bladder movements- alternate
Addictions:
Used to drink alcohol and also there is h/o smoking but stopped since 4yrs.
FAMILY HISTORY:
No significant family history
GENERAL AND PHYSICAL EXAMINATION:
Patient is conscious,coherent,cooperative
No signs of pallor,icterus,cyanosis,clubbing,lymphadenopathy
B/L pedal edema +ve
VITALS:
Temperature-Afebrile
PR-84bpm
BP-140/90mm Hg
RR-20cpm
SPO2-98% at RA
GRBS-84mg/dl
SYSTEMIC EXAMINATION:
CVS examination:
No visible pulsations, scars, engorged veins. No rise in jvp
Apex beat is felt at 5 Intercoastal space medial to mid clavicular line.
S1 S2 heard . No murmurs.
Respiratory system :
Shape of chest is elliptical, b/l symmetrical.
Trachea is central. Expansion of chest is symmetrical
Bilateral Airway Entry - positive
Normal vesicular breath sounds
Per Abdominal examination:
Soft , non tender
bowel sounds heard
CNS examination:
No focal neurological deficit
Normal speech
PROVISIONAL DIAGNOSIS:
-Anaemia secondary to ?CKD
-AKI on CKD
-Right lower limb venous insufficiency
-Denovo HTN
-K/C/O type 2 DM since 12yrs
-Esophageal candidiasis
-Grade 1 prostatomegaly
-?Neurogenic bladder
Upon admission patient was taken for surgery cross consultation on 06/09/23 i/v/o non healing wound over right foot and they diagnosed as ulcer over ventral aspect of 3rd right toe and they prescribed:
-Tab.Augmentin 625 mg po/Bd
-Tab.Pan 40mg po/od
-continue rest of the treatment as per physician orders
-review with reports
He was also taken for Gastroenterology cross consultation on 08/09/23 i/v/o severe anaemia (?) upper GI bleed and they diagnosed as oesophageal candidiasis with no upper GI bleed.
They prescribed capsule.Fluconazole 100mg po/Bd for 5 days
He was also taken for urology cross consultation on 08/09/23 i/v/o unable to pass urine since 1day
-dribbling of urine +
-burning micrurition +
-H/o frequency + ,10 times/day
-H/o urgency +
-H/o poor stream of urine + (1week) and distension of lower abdomen for which foleys catheterisation was done and removed 2days back
They diagnosed it as acute retention of urine with grade 1 prostatomegaly with DM, ?Neurogenic bladder
Foleys catheterisation was done —on foleys catheterisation 1200ml urine output noticed.
They prescribed:
-Tab.Tamsulosin 0.4mg po/hs
-Syp.Alkastone B6 10ml in 1/2 glass of water po/Bd
-Syp.Cremaffin 10ml po/hs
-do not remove foleys
-review to urology opd after 3weeks on monday/thursday
TREATMENT:
1)Inj.Mixtard sc/bd (25units in morning,25units in evng)
2)Inj.Pan 40mg iv/od
3)Tab.Augmentin 625mg po/bd
4)Tab.Nodosis 500mg po/bd
5)Tab.Shelcal ct po/od
6)Tab.Nicardia 20mg po/bd
7)Tab.Lasix 40mg po/bd
8)Tab.orofer xt po/od
9)Capsule.Fluconazole 100mg po/bd
10)Tab.Tamsulosin 0.4mg po/hs
11)Syp.Alkastone b6 15ml in 1glass of water po/bd
ECG:
X-RAY RIGHT FOOT OBLIQUE VIEW:
X-RAY RIGHT FOOT AP VIEW:
CHEST X-RAY PA VIEW:
USG CHEST:
On 04/09/23
04/09/23
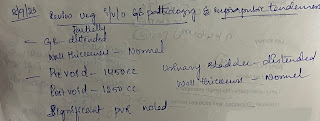
07/09/23
2D ECHO:
On 04/09/23
















Comments
Post a Comment