Hall ticket number 1701006131; N.JOSHUA PAUL, long case.
50/M FEVER COUGH WITH SPUTUM,UNCONTROLLED SUGARS
CHIEF COMPLAINTS
HOPI
Fever since 12-days high grade-not associated with chills and rigor, evening rise is seen associated with sweating
Cough since 7- days associated with less amount of sputum, mucoid, blood tinged aggravated on changing position from lying down to sitting position, no releiving factors
SOB grade - I MMRC -: 7 days, more associated with cough, relieved on rest not associated with wheeze
H/o RTA 1 1/2 year back
Fracture of neck of left femur with dynamic hip screw surgery done in another Hospital.Immobilisation 1-1/2 year back
DAILY ROUTINE
Patient wakes up at 5:30 am, freshens up, takes his diabetic tab glimiperide, drinks tea at 7 am, eats breakfast (Rice) at 9am and due to his past RTA from 2yr back, had fracture near lateral part of upper thigh placement of rod implant was done. Since then he is not going to farming and stays at home.At 1:00 pm he takes lunch(Rice) and walks a few steps in house then sleeps for an hour. Eats dinner(Rice) at 9:00 pm and goes to sleep by 10:00pm.
PERSONAL HISTORY
Patient is an Alcoholic and Smoked 18 cigarettes a day. later he started smoking Beedi Suttas(high tobacco cigar) in day.
Patient attendant said that their neighbour has TB ( who is son in law of him )
And Patient visits weekly 4 times to his home & spend with him approximately 1-hour a day
Patient started to have fever since 10 days at night time with burning sensation all over the body
Patient started to have unbearable pain at lower back during cough and always needed help from attendants to hold his back during coughing.
Diet is mixed
PAST HISTORY
K/c/o DM since 2 years was diagnosed during his RTA treatment and is on regular Glimipride 1mg &Metformin 500mg medication since then.
He has no history of hypertension, diabetes ,asthma, epilepsy, tuberculosis.
GENERAL EXAMINATION
Patient is conscious, cooperative ,coherent and oriented with time , place , date.
Slight pallor is seen,
No icterus, cyanosis, clubbing, lymphadenopathy, edema was noted
VITALS:
Bp- 90/80mm Hg
Pr-90 bpm
Rr-25 cpm
Temperature:99.5
Spo2: 98%@RA
GRBS- 112mg/do
Sputum sample:
Burns in both hands:
Slight discoloration on lower back:
Surgical implant (L) Leg scar:
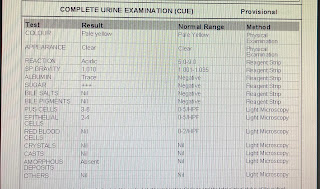
INVESTIGATIONS
06.05.2023
07.06.2023
HRCT - Findings
06.06.2023
Urine for culture
SYSTEMIC EXAMINATION
CVS:S1 S2 heard , No murmurs
CNS: No focal neurological deficit
Respiratory system :
Inspection: shape of chest is flat with bilaterally symmetrical movements
RR: 20cpm
Type of breathing : abdominothoracic
No supraclavicular hollowing or crowding of ribs seen, no visible sinus or scars
Palpation : no local rise of temperature seen, no tenderness
Position of trachea is central without any deviation
Tactile vocal fremitus : increased in the left upper lobe.
Percussion : dull note on the left upper lobe
Auscultation : crepts heard
PROVISIONAL DIAGNOSIS
TREATMENT
IV Fluids@ 75ml /hr
Inj.Neomol 1gm IV/SOS (if temp more than 101 F)
Tab.Dolo 650mg PO/TID
Syp.Grillinctus dx 2tsp PO/TID
Inj HAI S/C TID ( acc to GRBS )
Inj Augmentin 1.2gm Iv/ BID until day 3 of admission
Tab Itraconazole 200mg Po/Tid





















































Comments
Post a Comment